HOW TO DEAL WITH PARKINSON’S DISEASE
Parkinson’s disease is a brain disorder that leads to shaking, stiffness, and difficulty with walking, balance, and coordination. Parkinson’s symptoms usually begin gradually and get worse over time. As the disease progresses, people may have difficulty walking and talking. They may also have mental and behavioral changes, sleep problems, depression, memory difficulties, and fatigue.

Both men and women can have Parkinson’s disease. However, the disease affects about 50 percent more men than women.
One clear risk factor for Parkinson’s is age. Although most people with Parkinson’s first develop the disease at about age 60, about 5 to 10 percent of people with Parkinson’s have “early-onset” disease, which begins before the age of 50. Early-onset forms of Parkinson’s are often, but not always, inherited, and some forms have been linked to specific gene mutations.
What Causes Parkinson’s Disease?
Parkinson’s disease occurs when nerve cells, or neurons, in an area of the brain that controls movement become impaired and/or die. Normally, these neurons produce an important brain chemical known as dopamine. When the neurons die or become impaired, they produce less dopamine, which causes the movement problems of Parkinson’s. Scientists still do not know what causes cells that produce dopamine to die.
People with Parkinson’s also lose the nerve endings that produce nor-epinephrine, the main chemical messenger of the sympathetic nervous system, which controls many functions of the body, such as heart rate and blood pressure. The loss of nor-epinephrine might help explain some of the non-movement features of Parkinson’s, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying-down position.

Many brain cells of people with Parkinson’s contain Lewy bodies, unusual clumps of the protein alpha-synuclein. Scientists are trying to better understand the normal and abnormal functions of alpha-synuclein and its relationship to genetic mutations that impact Parkinson’s disease and Lewy body dementia.
Although some cases of Parkinson’s appear to be hereditary, and a few can be traced to specific genetic mutations, in most cases the disease occurs randomly and does not seem to run in families. Many researchers now believe that Parkinson’s disease results from a combination of genetic factors and environmental factors such as exposure to toxins.
Symptoms of Parkinson’s Disease
Parkinson’s disease has four main symptoms:
- Tremor (trembling) in hands, arms, legs, jaw, or head
- Stiffness of the limbs and trunk
- Slowness of movement
- Impaired balance and coordination, sometimes leading to falls
Other symptoms may include depression and other emotional changes; difficulty swallowing, chewing, and speaking; urinary problems or constipation; skin problems; and sleep disruptions.
Symptoms of Parkinson’s and the rate of progression differ among individuals. Sometimes people dismiss early symptoms of Parkinson’s as the effects of normal aging. In most cases, there are no medical tests to definitively detect the disease, so it can be difficult to diagnose accurately.
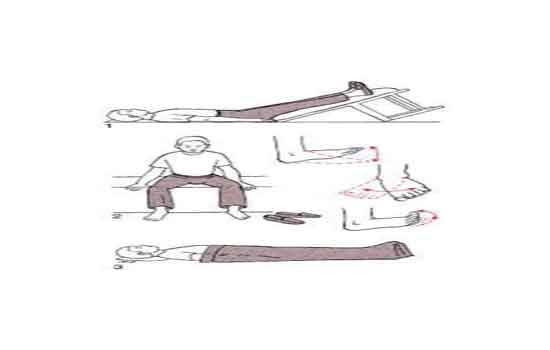
Early symptoms of Parkinson’s disease are subtle and occur gradually. For example, affected people may feel mild tremors or have difficulty getting out of a chair. They may notice that they speak too softly or that their handwriting is slow and looks cramped or small. Friends or family members may be the first to notice changes in someone with early Parkinson’s. They may see that the person’s face lacks expression and animation, or that the person does not move an arm or leg normally.
People with Parkinson’s often develop a parkinsonian gait that includes a tendency to lean forward, small quick steps as if hurrying forward, and reduced swinging of the arms. They also may have trouble initiating or continuing movement.
Symptoms often begin on one side of the body or even in one limb on one side of the body. As the disease progresses, it eventually affects both sides. However, the symptoms may still be more severe on one side than on the other.
Many people with Parkinson’s note that prior to experiencing stiffness and tremor, they had sleep problems, constipation, decreased ability to smell, and restless legs.

Diagnosis of Parkinson’s Disease
A number of disorders can cause symptoms similar to those of Parkinson’s disease. People with Parkinson’s-like symptoms that result from other causes are sometimes said to have Parkinsonism. While these disorders initially may be misdiagnosed as Parkinson’s, certain medical tests, as well as response to drug treatment may help to distinguish them from Parkinson’s. Since many other diseases have similar features but require different treatments, it is important to make an exact diagnosis as soon as possible.
There are currently no blood or laboratory tests to diagnose non-genetic cases of Parkinson’s disease. Diagnosis is based on a person’s medical history and a neurological examination. Improvement after initiating medication is another important hallmark of Parkinson’s disease.
Treatment of Parkinson’s Disease
Although there is no cure for Parkinson’s disease, medicines, surgical treatment, and physical therapies can often relieve some symptoms.
Rehabilitation:

Rehabilitation includes various therapies such as physical therapy, occupational therapy, speech therapy etc according to the condition of the patient. Which help with gait and voice disorders, tremors and rigidity, and decline in mental function. Other supportive therapies include a healthy diet and exercises to strengthen muscles and improve balance
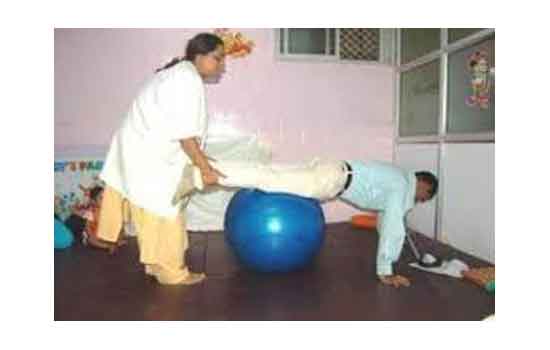
Blossom Rehabilitation center offer specialized services for people with Parkinson’s disease. Unlike an acute care hospital, where most treatment and monitoring is provided at the bedside, people in the program at Blossom Rehabilitation actively participate in daily treatment sessions. The length of Rehabilitation treatment varies depending on a person’s medical and rehabilitation needs.
Physiotherapy–
Physiotherapy aims to keep you moving safely and independently, with your body in as good a working condition as possible. A physiotherapist (also known as a physical therapist) is often a member of the multidisciplinary team, that is, a group of professionals with different areas of expertise, who together will help you manage your symptoms and maximize your quality of life.

Physiotherapists use exercise and other forms of physical therapy to help you keep your functional independence.
The key aims of physiotherapy in Parkinson’s are:
- maintain and improve functional ability and independence
- correct and improve posture and balance
- minimise the risk of falls
- allow strength and flexibility to be maintained
- enhance daily activities (getting in and out of bed, rising from a chair)
- maintain a safe walking pattern (with or without mobility aids)
- freezing is evident, coping strategies such as auditory or visual cues may be taught
- improve manual activities (reaching and grasping)
- maintain respiratory function through breathing exercises
- teach relaxation techniques
In Parkinson’s, the goals of physiotherapy will vary according to the phase of Parkinson’s being experienced.
Early stage:
The key aim in the early stage of the condition is to prevent inactivity and to improve physical ability in terms of aerobic capacity, muscle strength and joint mobility. Your physiotherapist may provide an exercise program that you can follow on your own or in a group, with suggestions and advice on maintaining your fitness levels.
Mid stage:
In this stage physiotherapy will aim to improve upper limb function, in particular reaching and grasping, as well as improving posture, balance, gait and transfers. Your physiotherapist may suggest a range of exercises to help with these activities, including hand exercises to help with manual dexterity so you can more easily button a shirt, for example. He or she may also collaborate with an occupational therapist to ensure that your home is safe and to reduce the risk of you falling.
Cueing strategies may also be suggested to improve gait and overcome freezing, cognitive movement strategies may be taught which allow you to break down complex movements into a sequence of individual movement that you can focus on following step by step, for example when transferring from a bed or a chair and you need to move to the edge, bend knees, place hands by your side to push up, lift your bottom etc.
Late stage:
In this stage, physiotherapy aims to prevent complications that may arise as a result of using a wheelchair or being bedridden. This includes maintaining your breathing, preventing pressure sores and working with careers to ensure that they position you correctly and avoid injuring themselves when lifting.
Physiotherapy and Cares
Physiotherapists can also advise your care and family how to help you stay as independent as possible. In addition, they can advise cares and family on ways to look after their own health, for example their back, if they help you with getting out of bed, chair or car.

Occupational therapy–
Occupational therapist will plan specialized therapeutic activities to handle daily activities at home and when outside. Special attention to be given with cues and safety training for activities of daily life.
Speech and swallow therapy–
Speech and language pathologist will work on improving speech and swallowing. Because this is very common in Parkinson’s patients and it has to cure with time and only done by speech rehabilitation.
Respiratory Therapy– Respiratory therapist will work to improve functioning of respiratory muscles
Nutrition counseling– Dietician can prescribe personalized diet based on the medical condition, drug-food interactions and preferences.
Psychosocial interventions– Clinical psychologist will manage general emotional wellbeing, depression and social isolation
Deep Brain Stimulation
For people with Parkinson’s who do not respond well to medications, deep brain stimulation, or DBS, may be appropriate. DBS is a surgical procedure that surgically implants electrodes into part of the brain and connects them to a small electrical device implanted in the chest. The device and electrodes painlessly stimulate the brain in a way that helps stop many of the movement-related symptoms of Parkinson’s, such as tremor, slowness of movement, and rigidity.
TREATMENT OF PARKINSONS WITH BEST PHYSIOTHERAPY CENTER IN DHKOLI..
Blossom physiotherapy center is one off leading rehabilitation center these days in dhkoli. And it is well equipped with ultra modular modalities. Dr.Jyoti Gupta (MPT pediatrics) that is a Pediatrics Physiotherapist as well as a certified Yoga instructor she complete her course from a well known YOGA ALLIANCE INTER NATIONAL FnY STUDIO is a head of the Blossom physiotherapy center and senior physiotherapist. She is having quite well exposure of various conditions and have good recovery rate. There is a huge team of other specialists who work as a team. They all are specialize in their field and apply their valuable knowledge in recovery of patient.

A Parkinson disease is progressive with time and produces other complications so, it is very important to take rehabilitation on time to avoid other difficulties. Physiotherapy help in preserve range of joint and avoid stiffness. But for that you need a well qualified and experienced physiotherapy doctor who helps you to regain motion without getting fatigue or muscular weakness. Moreover in this era of pandemic they provide proper hygiene treatment with maintenance of social distance. I recommend you to visit one time and feel the difference. For further information login to…..http:/www.blossomphysitherapy.in/



